With the 2018 ICD-10-CM and CPT® changes now released and in effect, cardiology is one of the specialties most impacted, with over 100 new, revised and deleted codes. There are also a few surprises that weren’t in the 2018 proposal, and that you may not have had much time to prepare for. It’s clear that, as a result, cardiology practices will be scrambling to comply, according to pathology compliance and coding expert Terry Fletcher.
Fletcher lays out the key cardiology-specific code changes—as well as the modifications to acute myocardial infarction (AMI) codes and Medicare updates—that represent new challenges for cardiology professionals as part of a Medical Coding Virtual Boot Camp with ProfEdOnDemand. There are changes this year in terms of the definition of “meaningful use,” as well as updates to HIPAA regulations. With her knowledge based on years of experience, Fletcher provides the concrete, practical information that providers and coders absolutely need to submit proper claims in 2018.
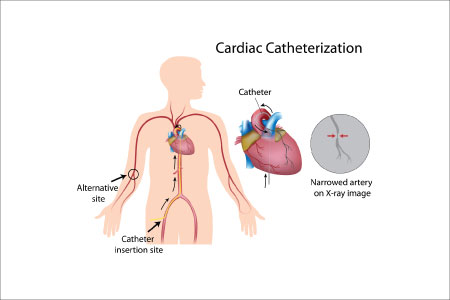
Don’t Confuse Catheter Codes
One helpful explanation Fletcher offers is the difference between often-confused procedures, such as catheterizations and angiographies.
Important: Both procedures involve the use of a catheter, but they are not identical, as one can be performed without the other. And there are three related codes that are regularly confused: 93454, 93458, and 93460. Each code involves the placement of a catheter in one or more coronary arteries for coronary angiography. What sets each apart is the following:
- 93454: no heart catheterization performed
- 93458: left heart catheterization (LHC) performed
- 93460: left and right heart catheterization performed
Fletcher further details what sets these procedures apart so you can feel confident knowing which code to use. As with always, check with each provider first if you have any doubts, but here are a couple basic tips to help differentiate:
- 93460 involves a left and right heart catheterization, while 93458 involves only an LHC.
- 93454 does not involve a catheterization, but instead simply a closure device angiography. Make sure you don’t code any closure devices separately, as they are included in this code.
What’s new for these codes for 2018 is that the CPT® handbook specifies that a cardiac catheterization prior to a percutaneous coronary intervention (PCI) cannot be reported unless it’s for a clear diagnostic purpose.
Bringing in the Modifiers
When reporting cardiology codes for 2018, be sure also that you understand the applications of modifiers -26 and -TC. These modifiers should be appended when billing only for the professional or technical aspect of a procedure, but not both. Any procedure with a “1” indicator in the Professional Component/Technical Component (PC/TC) field on the Medicare Physician Fee Schedule Database (MFSDB) is eligible for either of these two modifiers. If reporting other modifiers at the same time, place -26 or -TC right after the code, and then the others.
Knowing when to bill for each modifier can be tricky. Modifier -TC should be used when the provider is billing only for the technical component of a service, or when the code does not encompass the technical component only.
Likewise, modifier -26 is appropriate when a physician is billing only for the professional component of the service, and when the code does not encompass the professional part of the service only. If a provider is billing for a global code, or if both technical and professional aspects were rendered by the same provider, then neither modifier may be used.
Failing to append these modifiers appropriately has resulted in around 1.7 million Clerical Error Reopenings (CER) each year when Medicare Part B providers failed to submit correct claims, according to Novitas. CERs cost both providers and Medicare time and money, not to mention the wait for Medicare to process the corrected claim.
Correct Billing Equals Content Practices
When the incorrect modifier is used, or when the correct modifier simply isn’t present on the claim, serious consequences can impede the smooth flow of your practice. At the end of the day, less time spent correcting errors means more patient time for physicians, while for coders it means more time to dedicate quality attention to each claim submitted.
Join Fletcher’s prerecorded webinar for detailed information that can help you keep your practice financially fit for the coming year.