You must’ve been aware of the new chronic care management CPT code 99490 for a few months now, but do you know how to report it?
Beginning Jan. 1, 2015, Medicare began paying for chronic care management (CCM). This recognition has come as a welcome change since care management is considered as one of the important components of primary care contributing hugely to better health and care for individuals. Medicare pays separately under the Medicare Physician Fee Schedule (PFS) under Current Procedural Terminology (CPT) code 99490, for non-face-to-face care coordination services furnished to Medicare beneficiaries with multiple chronic conditions.
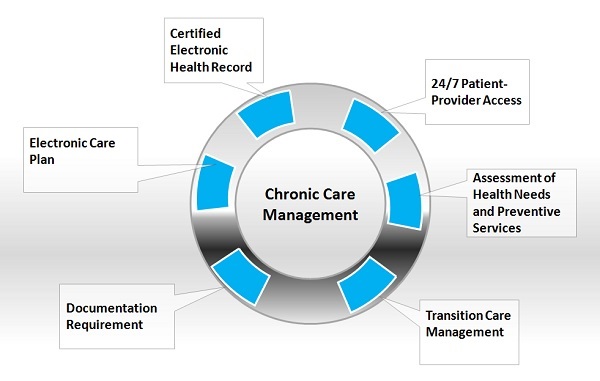
According to CMS, the CPT Code—99490— pays for clinical staff time directed by a physician or other qualified healthcare professional, per calendar month, with the following elements:
- At least two chronic conditions that are expected to last at least 12 months or until the death of the patient;
- Chronic conditions that place the patient at significant risk of death, acute exacerbation/decompensation, or functional decline; and
- When comprehensive care plan is established, implemented, revised, or monitored.
Reporting Chronic Care Management
You will have to meet few essential criteria to report the chronic care management, or you won’t be able to bill the services.
Certified Electronic Health Record (EHR)
You need to use a certified EHR to record problems, demographics and medications. Additionally, you will need to build a clinical summary record using a certified EHR.
24/7 Patient-Provider Access
Nonstop patient-provider access is essential to address urgent chronic care needs at all times.
Assessment of Health Needs and Preventive Services
Systematic assessment of health needs will ensure that the patient doesn’t miss out on any medical assessment, and that they receive preventive services on time.
Transition Care Management
Managed care transitions between health care providers, hospital, nursing facility and ER providers. “There are two pieces of this element: A certified EHR technology requirement to create and format the clinical summary you’d be exchanging with other providers, and managing care transitions using CCM certified technology,” says Ann Marshall, MSPH, of CMS’s division of practitioner service.
Electronic Care Plan
Electronic care plan requires the systematic creation and maintenance of a complete plan of care for all patient-centered health issues. A written or electronic copy of the care plan should be given to the patient or the care-giver, and also you need to document the care plan in the EHR using the CCM-certified technology. There is no specific format for 2015; however, you need to capture the care plan information and make it available on a 24/7 basis to all practitioners in the practice.
Documentation Requirement
The patient’s written consent needs to be documented along with authorization in the EHR using CCM-certified technology. This will make sure that the patient understands his eligibility for CCM and that you have the patient’s written consent to electronically share protected health information with other providers.
The CMS answered several pressing questions on CCM reporting during a webinar few months back. Also, at ProfEdOnDemand, expert speaker Kim Garner-Huey, MJ, CPC, CCS-P, PCS, CPCO, will help participants navigate documentation requirement for Primary Care Physician in TCM and CCM in an informative audio session.